| Message: 1. THERE'S LITTLE ROOM TO SPARE IN THE CRANIUM
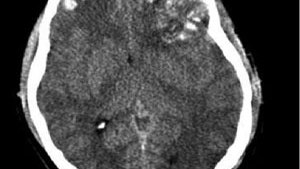
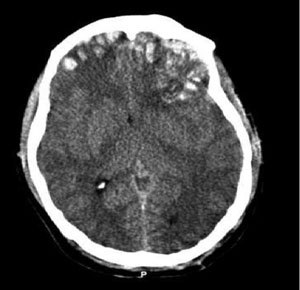
TBI can cause inflammation and swelling or bleeding from damage to brain tissue and blood vessels. Bleeding may occur within the brain (an intracranial hemorrhage) or the protective layers that surround it, such as an epidural, subdural or subarachnoid hemorrhage.
TBI can cause inflammation and swelling or bleeding from damage to brain tissue and blood vessels.
TBI can cause inflammation and swelling or bleeding from damage to brain tissue and blood vessels. (Photo courtesy of Rehman T, Ali R, Tawil I, Yonas H)
RELATED ARTICLES
Stroke: 10 things you need to know to save lives
STEMI: 10 things you need to know to save lives
Trauma: 10 things you need to know to save lives
The brain is tightly enclosed within the skull. Bleeding and inflammation cause a rise in intracranial pressure (ICP), which squeezes and damages brain structures, within that space. As ICP increases, sections of the brain may shift to different areas within the skull, or into the opening where the spinal cord enters the cranium, through a process known as herniation. The higher and longer ICP rises, the degree of permanent disability and likelihood of death increases.
Signs of increased ICP include altered mental status, unequal or nonreactive pupils, posturing, or seizures, as well as bradycardia and hypertension (Cushing's Phenomenon).
2. SLOW DOWN THE DAMAGE FROM SECONDARY BRAIN INJURY
Brain tissue does not regenerate, thus damage from the initial insult is generally permanent. The subsequent edema and bleeding from the primary injury then spreads to damage other areas of the brain, and treatment is aimed at limiting this secondary injury. Through airway protection, oxygenation or ventilation, blood pressure maintenance, and transport to a trauma center, EMS plays a vital role in stopping this cascade.
3. HEAD INJURED PATIENTS ARE UNRELIABLE HISTORIANS
Patients with TBI may be confused, combative, or unresponsive. They may be unable able to follow commands or report pain, and concurrent drug or alcohol intoxication makes assessment even more difficult. Assume that altered mentation is caused by a head injury instead of intoxication.
Rely on inspection, auscultation, and palpation to rule in other injuries, such as a change in the patient's facial expression when their abdomen is palpated. Remember that internal injuries cannot be ruled out, particularly those involving the spinal cord, so take spinal precautions in any patient with a head injury and altered mental status.
4. SOUND THE ALARM AT THE TRAUMA CENTER
Treatment for head-injured patients requires rapid assessment, imaging with a CT scan, and possibly neurosurgery. Time is brain, and the chance of disability or death increases with any delay.
Transporting patients to trauma centers that offer neurological services, and early activation of teams at these centers, streamlines the process to definitive care. Know which hospitals these are, initiate transport as quickly as possible, and alert the hospital to prepare staff and equipment for your arrival.
5. AIRWAY COMPROMISE FROM TBI COMES IN MANY FORMS
Unconscious head-injured patients may lose muscle tone in their jaw, and their tongue may obstruct the airway. The gag reflex may also be compromised in TBI patients, which increases the risk of aspiration from vomit or blood. Clenched teeth, known as trismus, is another common finding that makes position and suctioning airway secretions difficult. Attempt to open the airway with a jaw thrust. Use an oral or nasal airway if the patient will tolerate it, position the patient on their left side to help prevent aspiration, and suction secretions.
Endotracheal intubation is the definitive airway management for TBI, often after sedation and paralysis with RSI. This procedure carries considerable risk, and whether it should be done by ground EMS crews is controversial. Remember that the goal for airway management should be to use the least invasive means to maintain a clear path for oxygenation and ventilation.
6. HYPOXIA AND HYPOTENSION ARE HARMFUL – EVEN FOR A SHORT TIME
Irreversible brain damage can occur in TBI patients after only four minutes of anoxia, which can be caused by a compromised airway, altered respiratory patterns from the head injury, or lung injury in multi-system trauma. Use pulse-oximetry, skin color, and respiratory rate to assess adequate oxygenation. Administer oxygen via nasal cannula, non-rebreather mask, or bag valve to maintain a pulse-ox reading of at least 95%.
Cerebral oxygen delivery is also compromised by hypotension, which is associated with poor outcomes after even transient episodes. Hypotension caused directly by a head injury is a rare and ominous finding; it is more often caused by shock associated with other injuries. Administer IV fluids and titrate blood pressure to 90 – 100 mmHG systolic in head injured patients who are hypotensive.
7. VENTILATING TOO FAST REDUCES BLOOD FLOW TO THE BRAIN
As harmful as hypoxia is in TBI, hypocapnea from excessive ventilation is harmful as well. A higher respiratory rate decreases the amount of CO2 in the blood, which triggers cerebral vasoconstriction and less oxygen delivery. Hyperventilation of head injuries has been associated with poor outcomes.
When assisted ventilation is necessary in isolated head injuries, follow your local protocols regarding use of end-tidal CO2 (EtCO2) monitoring for a head-injured patient.
Shock from multisystem trauma can also cause a low EtCO2 reading, in which case it should not be used to guide ventilation. If capnography is not available, or if the patient may be in shock from other injuries, ventilate adults at 10 breaths per minute. There is one exception...
8. HYPERVENTILATION MAY SLOW HERNIATION
In cases of suspected ICP being so high that portions of the brain may be shifting out of the cranium, the benefit of temporarily reducing cerebral blood with mild hyperventilation may outweigh the harm from less oxygen delivery. Hyperventilation is ONLY indicated for patients who are posturing or have no motor response, have unequal or dilated and nonreactive pupils, or bradycardia and hypotension. Titrate the respiratory rate to maintain an EtCO2 reading between 30 and 35 (in the absence of multi-system trauma), or 20 breaths per minute.
9. YOU MAY HAVE A CONCUSSION
A concussion is a transient change in mentation after blunt head trauma. It can cause retrograde amnesia, and patients often repeatedly ask the same question after being given an answer. It can also cause a temporary loss of consciousness, disorientation, incoherent speech, or lack of coordination. Diagnosis of a concussion is made after a CT scan shows no structural abnormalities associated with these symptoms - not in the field.
While concussion symptoms typically resolve after a few hours or days, severe or multiple concussions can cause headaches, dizziness, depression, and difficulty concentrating for weeks. Especially worrisome is a secondary impact syndrome, where a patient sustains a second concussion before recovering from the first. This can cause rapid cerebral edema and herniation, and has a high mortality rate. Athletes with a head injury should not return to play until after symptoms have completely resolved.
10. BE ON THE LOOKOUT FOR BLOOD THINNERS
Patients taking blood thinners, including Coumadin and Plavix, are at risk of severe bleeding into the brain from relatively minor head injuries. Learn what medications these are, and factor the patient's medication list into your assessment. Signs and symptoms of intracranial bleeding may be delayed, especially in elderly people.
Assume that an altered mental status is a change from baseline unless proven otherwise, and perform a cranial nerve exam to detect subtle signs of closed head injury. Any patient taking a blood thinner who bumps their head should be evaluated at the hospital, no matter how minor their injury appears.
BONUS: AN OUNCE OF PREVENTION CAN SAVE A TON OF HEADACHES
Promoting bike helmet use is one way for EMS agencies to prevent the need to encounter one of the situations listed above. EMS providers are also at risk for head injuries in the back of a moving ambulance. Helmet use is standard in helicopters, and EMS-specific helmets are now available for use on ground ambulances. Consider how easily a concussion may occur from even a minor ambulance crash, and how easily they can be prevented. |