|
Αρχειοθήκη ιστολογίου
-
►
2023
(138)
- ► Φεβρουαρίου (74)
- ► Ιανουαρίου (64)
-
►
2022
(849)
- ► Δεκεμβρίου (61)
- ► Σεπτεμβρίου (74)
- ► Φεβρουαρίου (65)
-
►
2021
(2936)
- ► Δεκεμβρίου (59)
- ► Σεπτεμβρίου (180)
- ► Φεβρουαρίου (325)
-
▼
2020
(1624)
- ► Δεκεμβρίου (293)
-
▼
Νοεμβρίου
(376)
-
▼
Νοε 25
(17)
- Extracellular vesicles-encapsulated microRNA-10a-5...
- A Multi-institutional Comparative Analysis of Prot...
- Feasibility and safety of exercise training and nu...
- Eradication of T-ALL cells by CD7 targeted univers...
- Starting dose selection and dose escalation for on...
- Risk factors, prognostic factors, and nomograms fo...
- The effect of postmastectomy radiotherapy in node-...
- Analysis of the expression and potential molecular...
- Benefit of dosimetry distribution for patients wit...
- Patients with pretreatment leukoencephalopathy and...
- Short-term mortality risks among patients with non...
- Predictive and prognostic role of tumour-infiltrat...
- Prediction of mortality in metastatic colorectal c...
- Toluidine blue versus frozen section for assessmen...
- Concurrent Dexamethasone Limits the Clinical Benef...
- FDA Approval Summary: Selpercatinib for the Treatm...
- Darolutamide: A Review in Non-Metastatic Castratio...
-
▼
Νοε 25
(17)
- ► Σεπτεμβρίου (234)
- ► Φεβρουαρίου (28)
-
►
2019
(13362)
- ► Δεκεμβρίου (19)
- ► Σεπτεμβρίου (54)
- ► Φεβρουαρίου (5586)
- ► Ιανουαρίου (5696)
-
►
2018
(66471)
- ► Δεκεμβρίου (5242)
- ► Σεπτεμβρίου (5478)
- ► Φεβρουαρίου (4835)
- ► Ιανουαρίου (5592)
-
►
2017
(44259)
- ► Δεκεμβρίου (5110)
- ► Σεπτεμβρίου (5105)
-
►
2016
(7467)
- ► Δεκεμβρίου (514)
- ► Σεπτεμβρίου (1038)
- ► Φεβρουαρίου (793)
Αναζήτηση αυτού του ιστολογίου
Τετάρτη 25 Νοεμβρίου 2020
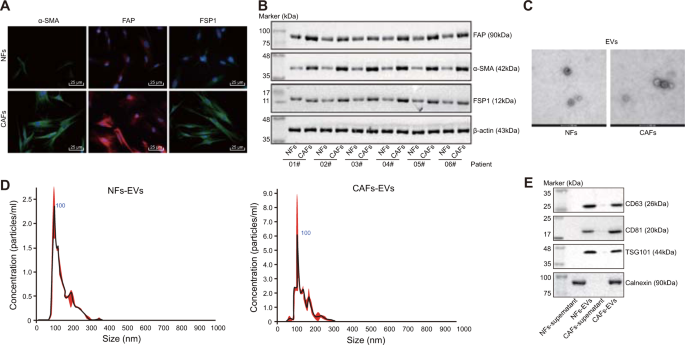
Extracellular vesicles-encapsulated microRNA-10a-5p shed from cancer-associated fibroblast facilitates cervical squamous cell carcinoma cell angiogenesis and tumorigenicity via Hedgehog signaling pathway
A Multi-institutional Comparative Analysis of Proton and Photon Therapy-Induced Hematologic Toxicity in Patients With Medulloblastoma
|
Feasibility and safety of exercise training and nutritional support prior to haematopoietic stem cell transplantation in patients with haematologic malignancies
|
Eradication of T-ALL cells by CD7 targeted universal CAR-T cells and initial test of ruxolitinib-based CRS management
|
Starting dose selection and dose escalation for oncology small molecule first-in-patient trials: learnings from a survey of FDA-approved drugs
|
Risk factors, prognostic factors, and nomograms for bone metastasis in patients with newly diagnosed infiltrating duct carcinoma of the breast: a population-based study
|
The effect of postmastectomy radiotherapy in node-positive triple-negative breast cancer
|
Analysis of the expression and potential molecular mechanism of interleukin-1 receptor antagonist (IL1RN) in papillary thyroid cancer via bioinformatics methods
|
Benefit of dosimetry distribution for patients with multiple brain metastases from non-small cell lung cancer by a Cyberknife stereotactic radiosurgery (SRS) system
|
Patients with pretreatment leukoencephalopathy and older patients have more cognitive decline after whole brain radiotherapy
|
Short-term mortality risks among patients with non-metastatic bladder cancer
|
-
This protocol presents an in vitro live-imaging phagocytosis assay to measure the phagocytic capacity of astrocytes. Purified rat astrocyt...
-
Measuring alterations in metabolic rates is central to understanding the progression of various diseases and aging. Here, we present a nov...
-
Synopsis Standards-based data management facilitates data preservation, discoverability, and access for effective data reuse within resear...